Have you ever been told that your snoring could wake the dead? Or perhaps you’ve experienced inexplicable daytime fatigue despite getting what you thought was a full night’s rest? For James Peterson, a 43-year-old marketing executive and father of two, these symptoms seemed like minor inconveniences—until the day he fell asleep at the wheel, narrowly avoiding a catastrophic accident. “That was my wake-up call,” James recalls. “What I thought was just normal tiredness nearly cost me everything.” His doctor’s diagnosis? Obstructive sleep apnea—a condition affecting an estimated 22 million Americans, with a staggering 80% of moderate to severe cases remaining undiagnosed.
Sleep apnea isn’t merely a nuisance that disrupts your night and annoys your partner. It’s a potentially life-threatening condition that repeatedly halts your breathing during sleep, sometimes hundreds of times per night, each interruption jolting your body from restorative deep sleep into a fight-or-flight stress response. These constant disruptions not only fragment your sleep but trigger systemic inflammation and strain your cardiovascular system. The long-term implications are sobering: untreated sleep apnea significantly increases your risk of high blood pressure, heart disease, stroke, type 2 diabetes, and even certain cancers. According to the American Academy of Sleep Medicine, the risk of death from all causes increases between two and three times in those with untreated severe sleep apnea.
Despite these alarming statistics, sleep apnea remains one of the most underdiagnosed conditions in modern medicine. Many sufferers attribute their symptoms to stress, aging, or simply being “a bad sleeper,” while physicians may miss the connection between sleep apnea and the cascade of health problems it creates. This critical gap in awareness and diagnosis means millions of Americans continue to suffer needlessly, their health silently deteriorating while an effective treatment remains just out of reach. In this article, we’ll explore the warning signs of sleep apnea, its profound health impacts, the latest diagnostic approaches, and treatment options that are transforming lives—perhaps even saving them.
Understanding Sleep Apnea: More Than Just Snoring
When Lisa Matthews’ husband recorded her sleeping, she was horrified by what she heard. “The snoring was bad enough, but the gasping and choking sounds terrified me,” she admits. “There were these long pauses where I wasn’t breathing at all, then these desperate gulps for air. It was like listening to someone drowning.” What Lisa was witnessing was the classic presentation of obstructive sleep apnea (OSA), the most common form of the disorder.
Sleep apnea comes in three primary forms, each with distinct mechanisms but similarly serious consequences. Obstructive sleep apnea occurs when throat muscles relax excessively during sleep, allowing soft tissues to collapse and block the airway. Central sleep apnea involves a failure of the brain to properly signal the breathing muscles, causing breathing to stop without any physical obstruction. Complex sleep apnea syndrome, also called treatment-emergent central sleep apnea, combines elements of both types.
The mechanics of obstructive sleep apnea are particularly insidious. When your airway narrows or closes completely, oxygen levels in your blood begin to fall. Your brain registers this emergency and partially wakes you, triggering a gasp or snort as your airway reopens. This cycle may repeat 5 to 30 times or more each hour throughout the night. Most sufferers remain unaware of these awakenings, experiencing only the downstream effects of chronically fragmented sleep.
Certain physical characteristics significantly increase your risk of developing sleep apnea. Excess weight is the most common risk factor, with fat deposits around the upper airway potentially obstructing breathing. According to a study published in the Journal of Clinical Sleep Medicine, approximately 70% of adults with OSA are overweight or obese. However, Dr. Michelle Rivera, a pulmonologist specializing in sleep disorders, emphasizes that normal-weight individuals aren’t immune: “We’re seeing increasing numbers of patients with completely normal BMIs who have significant sleep apnea due to craniofacial structure, enlarged tonsils, or neuromuscular factors.”
Age represents another significant risk factor, with OSA prevalence increasing substantially after age 40. Men are diagnosed with sleep apnea approximately two to three times more frequently than women, though this gap narrows after menopause. Family history also plays a role, with genetic factors influencing both airway anatomy and respiratory control.
Additional risk factors include smoking, which increases inflammation and fluid retention in the upper airway; nasal congestion from allergies or anatomical abnormalities; and use of sedatives, alcohol, or other substances that relax throat muscles. Medical conditions including hypothyroidism, acromegaly, and Parkinson’s disease can also contribute to sleep apnea development.
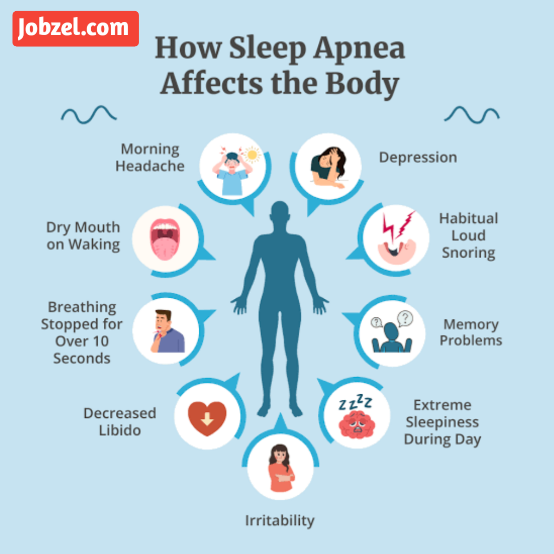
The symptoms of sleep apnea extend far beyond nighttime disturbances. While loud snoring, gasping during sleep, and observed breathing interruptions represent the most visible manifestations, many sufferers first notice daytime symptoms. These include excessive daytime sleepiness, morning headaches, difficulty concentrating, irritability, and mood disturbances. “Many patients come to me after being treated for depression or attention problems for years,” notes neurologist Dr. James Chen. “When we address their underlying sleep apnea, these cognitive and psychological symptoms often improve dramatically.”
Perhaps most concerning is the relationship between sleep apnea and other serious health conditions. Each apnea event triggers a surge in stress hormones, elevates blood pressure, and increases blood sugar levels. Over time, this creates a perfect storm for cardiometabolic disease. Research published in the New England Journal of Medicine found that moderate to severe sleep apnea increases the risk of heart failure by 140%, stroke by 60%, and coronary heart disease by 30%. Additional studies have established links between untreated sleep apnea and atrial fibrillation, treatment-resistant hypertension, and worsening diabetes control.
As sleep medicine specialist Dr. Sophia Williams explains, “Sleep apnea isn’t just a sleep disorder—it’s a systemic condition that affects virtually every organ system. When patients ask me why diagnosis and treatment matter, I explain that we’re not just improving their sleep; we’re potentially adding years to their life.”
The Diagnostic Journey: From Suspicion to Certainty
For Robert Torres, a 56-year-old construction supervisor, the path to diagnosis began with his annual physical. “My blood pressure was through the roof despite two medications. When my doctor asked about my sleep, I laughed it off—I’d been a loud snorer for decades. But when he asked about daytime fatigue and morning headaches, something clicked. Those symptoms had become my normal, but they weren’t normal at all.”
The diagnostic journey for sleep apnea typically begins with recognition of key warning signs. While loud, chronic snoring remains the most common red flag, other indicators include witnessed breathing pauses, gasping or choking during sleep, excessive daytime sleepiness, morning headaches, difficulty concentrating, mood changes, increased nighttime urination, and sore throat or dry mouth upon waking. The presence of risk factors—obesity, advanced age, family history, or craniofacial abnormalities—further increases suspicion.
Initial screening often employs standardized questionnaires designed to assess sleep apnea risk. The STOP-BANG questionnaire (evaluating Snoring, Tiredness, Observed apnea, high blood Pressure, Body mass index, Age, Neck circumference, and Gender) and the Epworth Sleepiness Scale (measuring daytime sleepiness across different situations) help physicians quantify symptoms and determine whether further testing is warranted. These simple screening tools have demonstrated remarkable effectiveness, with the STOP-BANG questionnaire showing 93% sensitivity for detecting moderate to severe sleep apnea when properly administered.
Definitive diagnosis traditionally required polysomnography—a comprehensive overnight sleep study conducted in a specialized laboratory. This gold-standard test monitors brain waves, blood oxygen levels, heart rate, breathing patterns, and limb movements throughout the night. “In-lab studies provide the most complete picture,” explains sleep technologist Maria Ramirez. “We’re collecting data from 18 or more channels simultaneously, allowing us to detect not just apnea events but other sleep disorders that might be present concurrently.”
However, recognition of the massive undiagnosed population has driven development of more accessible testing options. Home sleep apnea tests (HSATs) now allow patients to undergo simplified testing in their own bedrooms. These devices typically monitor breathing patterns, oxygen levels, heart rate, and movement, though they collect less comprehensive data than laboratory polysomnography. “Home testing has revolutionized access to diagnosis,” says Dr. William Parker, medical director of a large sleep medicine practice. “We’ve reduced waiting times from months to days, dramatically lowered costs, and made testing available to patients who couldn’t or wouldn’t spend a night in a sleep lab.”
The American Academy of Sleep Medicine now recommends home sleep apnea testing as an appropriate diagnostic alternative for patients with a high pretest probability of moderate to severe obstructive sleep apnea without significant comorbidities. However, laboratory testing remains essential for complex cases, patients with comorbid medical conditions, or when initial home testing results are negative despite strong clinical suspicion.
Interpretation of sleep studies focuses on the apnea-hypopnea index (AHI)—the average number of breathing disruptions per hour of sleep. An AHI below 5 is considered normal, while 5-15 indicates mild sleep apnea, 15-30 moderate sleep apnea, and above 30 severe sleep apnea. Additional metrics including oxygen desaturation frequency and depth, sleep architecture disruption, and presence of central apnea components further refine the diagnosis and guide treatment decisions.
Insurance coverage for sleep apnea testing has expanded significantly in recent years, with most major carriers now covering both laboratory and home testing when properly ordered. Medicare covers sleep testing for beneficiaries with symptoms suggestive of sleep apnea and specific clinical conditions, though specific documentation requirements apply. With home testing options typically costing $200-500 (compared to $1,000-3,500 for laboratory polysomnography), financial barriers to diagnosis have decreased substantially.
“The biggest obstacle to diagnosis isn’t access or cost anymore—it’s awareness,” emphasizes Dr. Rivera. “Both patients and many primary care providers still don’t recognize the severity and prevalence of this condition. We need to normalize sleep evaluations as a routine part of preventive care, especially for those with risk factors or symptoms.”
Treatment Options: Finding Your Path to Better Sleep and Health
After fifteen years of progressively worsening sleep quality, Vincent Chambers finally underwent a sleep study at his wife’s insistence. His AHI of 38—indicating severe sleep apnea—shocked him. “I had no idea I was essentially choking 38 times every hour throughout the night,” he recalls. “No wonder I felt terrible all the time.” But Vincent’s story takes an uplifting turn. “Within three days of starting CPAP therapy, I felt like a different person. The brain fog lifted, my energy returned, and for the first time in years, I actually remembered my dreams. It wasn’t just a treatment—it was a second chance at life.”
Effective treatment options for sleep apnea have expanded significantly in recent years, ranging from lifestyle modifications to advanced medical devices and surgical interventions. The appropriate approach depends on apnea severity, underlying causes, patient preferences, and comorbid conditions.
Positive airway pressure (PAP) therapy remains the gold standard treatment for moderate to severe sleep apnea. These devices deliver pressurized air through a mask worn during sleep, creating a pneumatic splint that prevents airway collapse. Continuous positive airway pressure (CPAP) provides a constant pressure level, while bilevel positive airway pressure (BiPAP) delivers higher pressure during inhalation and lower pressure during exhalation. Auto-titrating PAP (APAP) devices dynamically adjust pressure throughout the night based on detected respiratory events.
Modern PAP devices bear little resemblance to the bulky, noisy machines of years past. “Today’s CPAP technology is remarkably sophisticated,” notes respiratory therapist Kevin Williams. “Units are compact, quiet, and equipped with comfort features like heated humidification, pressure ramp-up, and pressure relief during exhalation. Many integrate with smartphone apps that provide detailed sleep data and coaching to improve therapy adherence.”
Adherence remains the primary challenge with PAP therapy, with studies indicating 30-50% of patients use their devices less than prescribed. Mask discomfort represents the most common complaint, but technological advances have dramatically expanded mask options. “Finding the right mask is crucial,” emphasizes sleep technologist Jennifer Rodriguez. “We now have dozens of designs ranging from full-face masks to nasal pillows that make minimal contact with the face. Many new users don’t realize that mask discomfort is usually solvable through proper fitting and selection.”
For patients with mild to moderate sleep apnea or those who cannot tolerate PAP therapy, oral appliances offer an effective alternative. These custom-fitted devices, designed by dentists with special training in sleep medicine, reposition the lower jaw and tongue to maintain airway patency during sleep. Research indicates they eliminate or significantly reduce breathing disturbances in 65-75% of patients with mild to moderate OSA.
Dr. Michael Thompson, a dental sleep medicine specialist, explains their appeal: “Oral appliances are silent, portable, and require no electricity. Many patients find them far less intrusive than PAP therapy, which significantly improves consistent usage. While they’re typically less effective than CPAP for severe apnea, for the right candidate they can be transformative.”
Surgical interventions target the specific anatomical issues causing airway obstruction. Traditional procedures include uvulopalatopharyngoplasty (UPPP), which removes excess tissue from the soft palate and throat; genioglossus advancement, which repositions the tongue attachment to prevent airway blockage; and maxillomandibular advancement, which moves both jaws forward to enlarge the airway space.
Newer, less invasive procedures have expanded surgical options. Hypoglossal nerve stimulation implants a small device that monitors breathing patterns and stimulates the nerve controlling tongue movement when necessary to maintain airway patency. “These implants represent a significant advancement for patients with moderate to severe OSA who cannot tolerate CPAP,” says otolaryngologist Dr. Rebecca Chen. “Success rates are impressive, with about 75% of carefully selected patients achieving significant improvement.”
For patients with mild sleep apnea or simple snoring, lifestyle modifications may suffice. Weight loss can substantially improve or even resolve sleep apnea in overweight individuals—studies indicate a 10% weight reduction can reduce AHI by up to 26%. Positional therapy helps those whose breathing problems occur primarily when sleeping on their backs. Avoiding alcohol and sedatives before bedtime, establishing regular sleep schedules, and treating nasal congestion can further reduce apnea severity.
Insurance coverage for sleep apnea treatments has improved substantially, with most plans now covering PAP therapy and necessary supplies with a valid diagnosis and prescription. Coverage for oral appliances typically requires documentation of PAP intolerance or preference for selected patients with mild to moderate disease. Surgical coverage varies more significantly by carrier and procedure type.
“The most important aspect of treatment is finding an approach the patient will actually use consistently,” emphasizes Dr. Williams. “The most advanced therapy is worthless if it sits unused. We’ve become much more collaborative in our approach, working with patients to find solutions that fit their lifestyle and preferences while effectively addressing their breathing disruptions.”
Living Well With Sleep Apnea: Beyond the Diagnosis
When Melissa Rodriguez was diagnosed with sleep apnea at 37, she initially saw it as yet another health problem to manage. “I felt defective,” she admits. “Here was another condition to add to my growing list.” But as treatment improved her sleep quality, her perspective shifted dramatically. “My ‘sleep disorder’ turned out to be the key to resolving issues I’d struggled with for years—my mood improved, my blood pressure normalized, and my energy levels soared. Addressing my sleep apnea didn’t just add another treatment to my routine—it simplified my entire health picture.”
A sleep apnea diagnosis represents the beginning of a journey toward improved health and well-being rather than an endpoint. Successful long-term management extends beyond initial treatment to encompass lifestyle modifications, consistent therapy use, regular monitoring, and integrated care across medical specialties.
The transformative health benefits of effective sleep apnea treatment extend throughout the body. Research published in the Journal of the American Medical Association demonstrated that CPAP therapy reduces 24-hour blood pressure measurements by an average of 2.5-3.5 mmHg, with more pronounced effects in patients with resistant hypertension. A landmark study in the New England Journal of Medicine found that CPAP treatment reduced cardiovascular events by 64% in patients with both coronary artery disease and sleep apnea. Additional research has documented improvements in insulin sensitivity, inflammation markers, cognitive function, mood stability, and quality of life measures.
Maximizing these benefits requires consistent, optimal therapy use. For PAP users, this means using the device whenever sleeping—including naps—for the entire sleep duration. Modern PAP machines provide detailed usage data including hours used, mask leak measurements, and residual breathing events. Regular review of this information with sleep specialists allows timely adjustments to improve both effectiveness and comfort.
“The first three months are critical for establishing long-term adherence,” notes sleep coach Thomas Jenkins. “We focus intensively on troubleshooting any barriers during this period—addressing mask discomfort, managing side effects like nasal congestion, and reinforcing the connection between treatment and improved daytime functioning. Once patients experience the benefits and develop a comfortable routine, consistent use becomes much easier to maintain.”
Integrating sleep apnea management with care for related conditions significantly improves outcomes for both. Cardiologists increasingly screen heart patients for sleep-disordered breathing, recognizing that untreated apnea can undermine cardiovascular treatments. Similarly, endocrinologists have found that addressing sleep apnea improves diabetes control. This coordinated approach requires effective communication between specialists and primary care providers.
Regular reassessment ensures treatment remains optimal as circumstances change. Weight fluctuations, aging, medication changes, and other factors can alter sleep apnea severity and treatment requirements. Most sleep specialists recommend annual follow-up for stable patients, with more frequent monitoring for those with complex conditions or adherence challenges.
Support resources have expanded dramatically with growing awareness of sleep apnea’s prevalence. Online communities connect patients with peers navigating similar challenges, while educational resources from organizations like the American Sleep Apnea Association provide evidence-based information for newly diagnosed individuals. Sleep medicine practices increasingly offer dedicated support programs with respiratory therapists, sleep coaches, or nurse educators who provide ongoing guidance beyond physician visits.
For those concerned about the lifetime commitment to therapy, emerging research offers hope. “We’re identifying specific patient subgroups who may benefit from time-limited interventions,” explains sleep researcher Dr. Sarah Martinez. “For example, some patients with mild to moderate OSA who achieve significant weight loss or undergo specific anatomical corrections may reduce their apnea severity to the point where continuous therapy is no longer necessary. Upper airway exercises developed by speech pathologists show promise in reducing apnea severity in selected patients. The future likely holds more personalized approaches based on each patient’s specific apnea mechanisms.”
For Melissa Rodriguez, effective management has become second nature. “My CPAP is as much a part of my bedtime routine as brushing my teeth,” she says. “The difference is that I actually look forward to it, knowing how much better I’ll feel the next day. The quality of life improvement makes any minor inconvenience completely worthwhile.”
Conclusion: The Wake-Up Call You Shouldn’t Ignore
Sleep apnea represents one of medicine’s most significant paradoxes—a serious, potentially life-threatening condition that remains chronically underdiagnosed despite effective treatment options. The consequences of this diagnosis gap are measured not just in quality of life, but in lives themselves. Every year, undiagnosed sleep apnea contributes to thousands of preventable deaths through increased cardiovascular events, motor vehicle accidents, and workplace incidents.
The good news is that awareness is growing. Primary care physicians increasingly recognize sleep-disordered breathing as a crucial health factor rather than a mere nuisance. Diagnostic technology has become more accessible and affordable. Treatment options have expanded to accommodate diverse patient needs and preferences. Insurance coverage has improved substantially. The path from suffering to treatment has never been more straightforward.
If you recognize the warning signs discussed in this article—chronic snoring, witnessed breathing pauses, excessive daytime sleepiness, morning headaches, or unexplained fatigue—don’t dismiss these symptoms as normal variations or inevitable consequences of aging or stress. A simple conversation with your healthcare provider can start you on the path toward diagnosis and treatment. For many patients, the appropriate question isn’t “Can I adapt to sleep apnea therapy?” but rather “How did I function for so long without it?”
Beyond individual health, addressing sleep apnea carries broader implications. Partners of sleep apnea sufferers often experience their own sleep disruption from snoring and concern about breathing pauses. Children and family members benefit from improved parental energy, mood, and engagement. Employers gain from reduced absenteeism and improved productivity. The ripple effects of effective treatment extend far beyond the individual patient.
What steps will you take if you suspect sleep apnea might be affecting your health or that of a loved one? Will you complete an online risk assessment, discuss symptoms with your doctor, or encourage a chronically snoring partner to seek evaluation? We invite you to share your experiences, questions, and concerns in the comments below or to reach out directly to sleep medicine resources in your community.
Sleep represents nearly a third of our lives and fundamentally shapes our waking experience. When sleep quality suffers, every aspect of health and functioning is compromised. By recognizing and addressing sleep apnea, you’re not just improving your nights—you’re transforming your days and potentially extending your years of healthy living. That’s a wake-up call worth heeding.